The JCNDE publishes a 30-page document that breaks down exactly what's on the INBDE. Every topic. Every weight. The official map to a 500-question exam.
It's free. It's public. And almost nobody actually uses it.
Some candidates have never opened it. Others downloaded it, skimmed the percentages, maybe highlighted "Oral Health Management: 42%"—then closed it and went back to grinding Qbanks.
Because what are you supposed to do with "Foundation Knowledge Area 6: General and disease-specific pathology"? How does knowing that "Diagnosis and Treatment Planning" is 36% change what you study tonight?
For most people, the official blueprint is something they know exists but have never actually used.
The blueprint isn't a study guide. It's a map. And a map is useless if you don't know how to read it.
The blueprint tells you categories. It doesn't tell you how a question about pulp pathology becomes a question about diabetes management. It doesn't explain why the exam feels harder than the content you studied. It lists biostatistics at 10%—but it doesn't tell you that's roughly 50 questions, or that most candidates barely touch the subject.
When's the last time you practiced a biostatistics question?
This guide translates the official specifications into study decisions you can actually make.
The Exam Your Seniors Took No Longer Exists
In 2022, 0.8% of US dental students failed the INBDE on their first attempt. Less than one in a hundred.
That number is now closer to 16%. One in six.
If you're an international dental graduate, the odds are even steeper—first-attempt failure rates between 16-39%, with over half failing on retakes.
Note for ITDs: The INBDE is required for U.S. licensure and U.S. advanced standing programs. If your goal is to practice in Canada, you need the NDEB Equivalency Process (AFK → ACJ → NDECC → Virtual OSCE) — not the INBDE.
The JCNDE raised the bar. The exam your D3 classmates took isn't the one you're sitting for. Last year's advice may already be outdated.
This is why the blueprint matters—it shows you exactly where those extra failure points are hiding.
Domains Don't Match Reality
The blueprint gives you three Clinical Content domains:
| Domain | Weight |
|---|---|
| Diagnosis and Treatment Planning | 36.2% |
| Oral Health Management | 42.0% |
| Practice and Profession | 21.8% |
Most candidates look at this and think: "Okay, I'll spend 42% of my time on clinical stuff, 36% on diagnosis, 22% on ethics and business." Then they create separate study blocks for each domain.
That approach backfires.
On the actual exam, a single question might count toward "Oral Health Management" in the scoring breakdown while requiring you to integrate knowledge from pharmacology, systemic pathology, and treatment planning. The domains describe how JCNDE categorizes questions, not how you'll experience them.
Example:
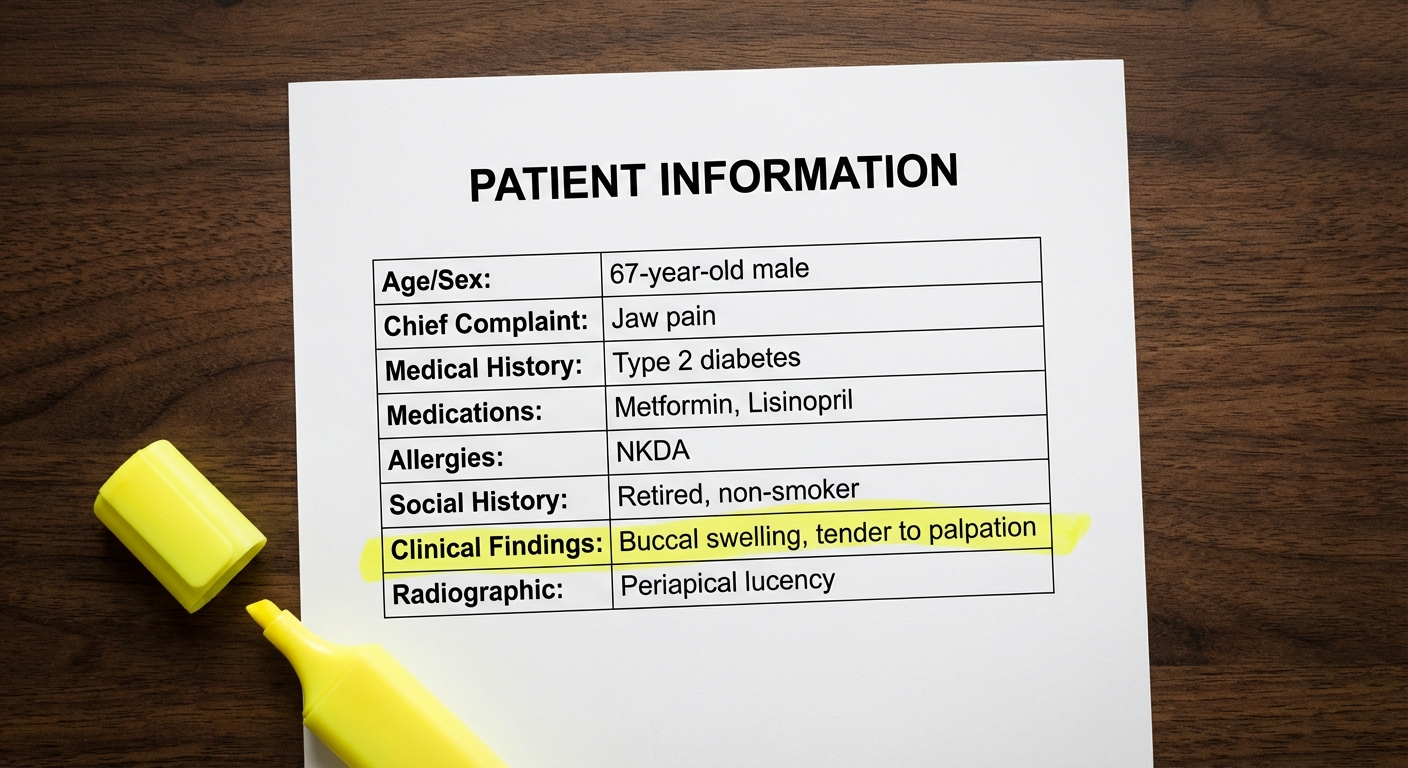
A 52-year-old patient with Type 2 diabetes and hypertension presents with a chief complaint of pain on chewing. Current medications include Metformin and Lisinopril. Clinical examination reveals a fractured amalgam restoration on tooth #30 with tenderness to percussion.
Which domain is this? Diagnosis and Treatment Planning—you're interpreting findings. Oral Health Management—you're deciding on treatment. But to answer correctly, you also need pharmacology (what are the implications of their medications?), pathology (what's causing the symptoms?), and possibly ethics (informed consent for treatment options).
Study subjects. Don't study domains.
The 10 Foundation Knowledge Areas—And the One Everyone Ignores
The Foundation Knowledge Document lists 10 areas that form the scientific backbone of every INBDE question:
| Code | What the Blueprint Says | What You Actually Need to Know |
|---|---|---|
| FK1 | Molecular, biochemical, cellular, systems-level development, structure and function | Anatomy, histology, embryology, physiology—the building blocks |
| FK2 | Physics and chemistry for normal biology and pathobiology | Biochemistry applied to clinical scenarios |
| FK3 | Physics and chemistry for technologies and materials | Dental materials—composites, cements, alloys |
| FK4 | Genetic, congenital, developmental diseases | Syndromes, risk assessment, developmental anomalies |
| FK5 | Immune and non-immune host defense mechanisms | Immunology, inflammation, wound healing |
| FK6 | General and disease-specific pathology | Oral pathology, systemic disease manifestations |
| FK7 | Biology of microorganisms | Microbiology—caries, perio pathogens, infections |
| FK8 | Pharmacology | Drugs, interactions, prescribing, anesthesia |
| FK9 | Behavioral Sciences, Ethics, Jurisprudence | Patient communication, consent, legal issues |
| FK10 | Research methodology, analysis, informatics | Biostatistics, study design, evidence-based practice |
Most candidates spend their time on FK1 through FK8. Anatomy, pathology, pharmacology—the "dental school" subjects.
FK10 is 9.8% of the exam.
That's roughly 49 questions on biostatistics and research methodology. One in ten.
Quick self-check: Have you spent one in ten of your study hours on sensitivity vs. specificity? On understanding p-values? On recognizing the difference between a cohort study and a case-control study?
Most candidates haven't. And those 49 questions show up whether you're ready or not.
The "I'll Skim It Later" Section That's 21.8% of Your Score
FK9 (Behavioral Sciences, Ethics, Jurisprudence) maps to the Practice and Profession domain. One in five questions.
You know how this usually goes: "I'll review HIPAA the night before. Ethics is common sense. I'll figure it out."
Then you're sitting in front of a question about whether a dental hygienist can administer local anesthesia under indirect supervision in a specific scenario, and you realize "common sense" doesn't tell you state practice act regulations.
What's actually in that 21.8%:
- HIPAA privacy rules (not just "keep patient info private"—specific scenarios)
- OSHA bloodborne pathogen standards
- Informed consent requirements and exceptions
- Scope of practice boundaries
- Risk management and documentation standards
- Practice management basics
- Ethical decision-making frameworks
These questions aren't ambiguous. There's a right answer based on established rules and regulations. The candidates who know the rules get them right. Everyone else guesses.
This Isn't the NBDE Anymore
The old NBDE rewarded memorization. Obscure facts. Random details that you crammed, regurgitated, and forgot.
The INBDE is different. From the INBDE Technical Report:
"The INBDE relies less on rote knowledge and information recall than the NBDE examinations do, and instead emphasizes the relevance of the basic sciences through test items that link science and clinical application."
Translation: They're not asking you to recall that Aδ fibers are myelinated and conduct at 6-30 m/s. They're asking you to explain why a patient's pain pattern suggests pulpal involvement rather than periodontal origin—and Aδ fibers are part of how you get there.
What This Looks Like on Exam Day
NBDE-era question:
Which nerve fibers are responsible for sharp, localized pain?
You either memorized "Aδ fibers" or you didn't. Four seconds to answer if you know it, random guess if you don't.
INBDE-era question:
A 45-year-old patient reports sharp, shooting pain in the lower right quadrant when drinking cold water. The pain is well-localized and lasts only seconds after the stimulus is removed. Which of the following BEST explains the neurophysiological basis for this pain pattern?
Same knowledge being tested—Aδ fibers. But now you have to recognize the clinical presentation (sharp, localized, brief, stimulus-dependent), connect it to the neurophysiology (Aδ fibers are myelinated, fast-conducting, low-threshold), and understand why the other options are wrong (C-fibers produce dull, aching, poorly localized pain—different clinical picture).
The candidate who memorized "Aδ = sharp pain" might still get this right. The candidate who understands why will get it right faster, without second-guessing.
Another Example: When Diabetes Shows Up in Perio
A patient with poorly controlled Type 2 diabetes presents for a routine exam. Clinical findings include generalized gingival inflammation and several sites with probing depths of 5-6mm. Which of the following systemic effects of the patient's condition is MOST directly contributing to the periodontal findings?
The trap answer: "Diabetes causes periodontal disease." That's true but useless—it doesn't answer which mechanism.
The right answer requires knowing that hyperglycemia leads to advanced glycation end products (AGEs), which impair neutrophil function and alter collagen metabolism. The periodontal destruction isn't just "diabetes = bad gums"—it's a specific pathophysiological process you need to identify.
On this exam, clinical and basic science aren't separate subjects. They're layered on top of each other in every question.
How to Read the Patient Box Without Wasting Time
Most INBDE questions come with a standardized patient presentation—the Patient Box. Per the INBDE Item Development Guide:
| Field | Information |
|---|---|
| Demographics | 45-year-old female |
| Chief Complaint | "My tooth hurts when I chew" |
| Medical History | Type 2 diabetes, hypertension |
| Medications | Metformin 500mg BID, Lisinopril 10mg daily |
| Allergies | Penicillin (rash) |
| Dental History | Last visit 2 years ago |
| Current Findings | BP 138/88, HR 72, afebrile |
| Images | Radiograph/clinical photos may be included |
Important: if a field isn't filled in, that information doesn't exist. Don't assume the patient has no allergies just because it's not mentioned. If the question doesn't tell you, you don't know. Answer based only on what's given.
A Reading Order That Works
You'll see hundreds of these boxes over two days. Reading them top-to-bottom every time is slow. Try this instead:
- Chief complaint first—what brought them in frames everything
- Demographics—age and sex narrow your thinking immediately
- Medical history + Medications—anything that changes your treatment approach?
- Allergies—penicillin allergy in a patient who needs antibiotics changes everything
- Clinical findings—now look at the actual data
With practice, you can pull the relevant information in 15 seconds instead of re-reading the same box three times.
300 Quick Hits, 200 Clinical Deep Dives
The exam splits into two formats:
| Question Type | Count | Percentage |
|---|---|---|
| Standalone Questions | 300 | 60% |
| Case-Based Questions | 200 | 40% |
These aren't just different question counts. They require different cognitive skills.
Standalone Questions (Day 1, Sections 1-3)
One question, one answer, move on. You might get a patient box, you might not. Everything you need is right there.
You have 105 minutes for 100 questions—about 63 seconds each. That's tight. If a question seems straightforward, it probably is. Don't talk yourself out of an obvious answer because you're looking for a trick. Answer, move on, flag if uncertain.
Case-Based Questions (Day 1 Section 4, All of Day 2)
A patient scenario with 3-6 questions attached. Dental charts. Periodontal charting. Radiographs. Clinical photos. Sometimes lab values.
The mistake most people make: starting to answer before finishing reading. Then question 4 references something from the initial presentation they skimmed over, and they have to re-read everything.
Read the whole case first. Build the clinical picture in your head. Then answer the questions. They often build on each other—what you figure out in question 1 might be relevant for question 3.
You have more time per question (105 minutes for 60-70 questions, roughly 90 seconds each), but the reading load is heavier. Use that time.
Day 2: Nothing But Cases
All 140 questions on Day 2 are case-based. Per the INBDE Candidate Guide:
| Section | Questions | Time | Format |
|---|---|---|---|
| Section 5 | 70 | 105 min | Case-based |
| Section 6 | 70 | 105 min | Case-based |
No standalone questions to break up the rhythm. No quick-hit items where you answer in 30 seconds and mentally recover. Four hours of reading patient scenarios, interpreting data, and synthesizing clinical pictures.
If you're mentally depleted from Day 1, this is where it shows. Reading comprehension slows when you're tired. Clinical reasoning gets fuzzy. The cases that would've taken you 4 minutes fresh now take 6 minutes exhausted—and you don't have that extra time.
What You're Actually Facing
A typical case might present:
- 62-year-old patient
- Chief complaint: loose lower front teeth
- Medical history: osteoporosis, oral bisphosphonates for 3 years
- Dental history: periodontal treatment 5 years ago
- Clinical: Class II mobility on mandibular incisors, generalized 4-5mm probing depths, radiographic bone loss
Questions attached to this case might cover:
- Diagnosis based on clinical and radiographic findings
- Risk factors contributing to the condition
- Treatment modifications given the bisphosphonate history
- Long-term prognosis
- Patient education priorities
Notice question 3. The bisphosphonate history sits in the medical section, easy to skim past. But it completely changes surgical decision-making (MRONJ risk). Miss that detail when reading the case, and you're stuck re-reading everything during question 3.
Different questions need different parts of the same case. You have to keep the whole picture accessible in your head.
Turning This Into a Study Plan
The blueprint gives you weights. Use them.
| Domain | Exam Weight | What This Means for You |
|---|---|---|
| Oral Health Management | 42% | ~210 questions. This is your biggest investment area. |
| Diagnosis and Treatment Planning | 36% | ~180 questions. Clinical reasoning, interpretation, treatment planning. |
| Practice and Profession | 22% | ~110 questions. The section everyone underprepares for. |
If you're spending 60% of your study time on clinical sciences and 5% on ethics/practice management, your allocation doesn't match the exam's allocation. Those 110 "soft" questions carry the same weight as the 110 hardest pathology questions.
Studying in Layers
When you're reviewing endodontics:
- What antibiotics would you prescribe? (pharmacology)
- Why does the pulp become necrotic? (pathology)
- How do you explain the procedure to an anxious patient? (behavioral science)
- What's your documentation protocol? (risk management)
When you're reviewing periodontics:
- How does diabetes affect periodontal outcomes? (systemic integration)
- What medications cause gingival enlargement? (pharmacology)
- What do you need for informed consent before surgery? (ethics/jurisprudence)
For every topic, ask yourself: what else connects to this? That's how the exam thinks.
The Biostatistics Checklist
You need these concepts cold:
- Study designs: RCT vs. cohort vs. case-control vs. cross-sectional—when to use each, what they can prove
- Sensitivity and specificity: What they measure, how they trade off
- PPV and NPV: How prevalence affects them
- Type I and Type II errors: What increases each risk
- P-values and confidence intervals: What they actually mean (not just "p < 0.05 is significant")
- Relative risk vs. odds ratio: When to use each
- NNT (Number Needed to Treat): How to interpret it
You won't calculate anything complex. You'll interpret results and evaluate whether a study's conclusions are valid. That's a learnable skill—but only if you actually study it.
What to Do With This
Reallocate your study time this week. If you haven't touched biostatistics, block out 10% of your remaining prep time for it. Not a skim-through—actual practice with sensitivity/specificity problems, study design identification, and interpreting research findings. Those 49 questions are coming whether you're ready or not.
Audit your "soft topic" coverage. Pull up your study tracker. How much time have you logged on ethics, HIPAA, informed consent, scope of practice? If the answer is "not much," you're gambling with 110 questions. These aren't subjective—they have right answers based on rules you either know or don't.
Change how you practice questions. When you get a clinical question wrong, don't just read the explanation and move on. Ask: what basic science concept was underneath this? What pharmacology was relevant? What would informed consent require here? Train yourself to see the layers.
Simulate Day 2 conditions. Before your exam, do at least one 140-question case-based session. No standalone questions to break it up. Time yourself. See how your comprehension holds up in hour three versus hour one. If it crashes, you've identified a problem you can fix before it costs you.
Practice reading patient boxes fast. Chief complaint first, then demographics, then medical history. Get to where you can extract what matters in 15 seconds. On 200+ case-based questions, that efficiency compounds.
The blueprint is a specification document. It tells you what's being tested, not how to study.
But now you know where the gaps are: the 10% on biostatistics that most people skip, the 22% on ethics and regulations they cram the night before, the integration that connects every clinical question back to basic science.
Most candidates who fail knew the material. They just didn't know the exam.